Q
In vitro fertilization (IVF) is a complex medical procedure used to assist individuals and couples in achieving pregnancy when they face difficulties conceiving naturally. This article will explore the IVF process, its indications, benefits, risks, and the advancements in this field.
Understanding IVF
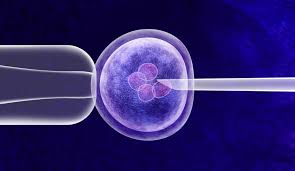
IVF is a type of assisted reproductive technology (ART) that involves the fertilization of an egg by sperm outside the body. The term “in vitro” translates to “in glass,” reflecting the laboratory environment where fertilization occurs. IVF can be performed using a woman’s own eggs and her partner’s sperm, or it may involve donor eggs and/or sperm.
The IVF Process
The IVF process typically consists of several key steps:
- Ovarian Stimulation: Hormonal medications are administered to stimulate the ovaries to produce multiple eggs instead of the single egg that usually develops each month. Monitoring through blood tests and ultrasounds helps assess the response.
- Egg Retrieval: Once the eggs are mature, a minor surgical procedure called transvaginal ultrasound aspiration is performed to retrieve the eggs from the ovaries. This procedure is usually done under sedation or anesthesia.
- Sperm Collection: A sperm sample is collected from the male partner or a donor. The sperm is then prepared and concentrated in the laboratory.
- Fertilization: The retrieved eggs are combined with the prepared sperm in a laboratory dish. Fertilization can occur naturally, or a single sperm may be injected into an egg through a process called intracytoplasmic sperm injection (ICSI).
- Embryo Culture: The fertilized eggs, now called embryos, are monitored for growth over several days. The embryologist assesses the quality of the embryos.
- Embryo Transfer: One or more healthy embryos are selected for transfer into the woman’s uterus. This is typically done through a thin catheter. Any remaining viable embryos may be frozen for future use.
- Pregnancy Test: Approximately two weeks after the embryo transfer, a blood test is performed to check for pregnancy.
Indications for IVF
IVF is recommended for various fertility issues, including:
- Blocked or Damaged Fallopian Tubes: This can hinder the passage of eggs and sperm.
- Ovulation Disorders: Conditions like polycystic ovary syndrome (PCOS) can affect ovulation.
- Endometriosis: This condition can impair fertility by affecting the reproductive organs.
- Male Factor Infertility: Low sperm count or motility may necessitate IVF.
- Unexplained Infertility: When no specific cause is identified after testing.
- Genetic Disorders: IVF can be combined with preimplantation genetic testing to avoid passing on genetic conditions.
Benefits of IVF
- Increased Chances of Conception: IVF can significantly increase the chances of conception, especially for couples with fertility challenges.
- Control Over Timing: Couples can plan the timing of pregnancy more effectively.
- Genetic Screening: Preimplantation genetic testing can help identify genetic disorders before pregnancy.
- Options for Same-Sex Couples and Single Parents: IVF allows for diverse family-building options.
Risks and Considerations
While IVF is generally safe, it does carry certain risks, including:
- Multiple Pregnancies: Transferring multiple embryos can lead to twins or more, which may pose health risks for both the mother and babies.
- Ovarian Hyperstimulation Syndrome (OHSS): Overstimulation of the ovaries can lead to swelling and pain.
- Ectopic Pregnancy: Rarely, an embryo may implant outside the uterus.
- Emotional and Financial Strain: The IVF process can be emotionally taxing and expensive, often requiring multiple cycles.
Advances in IVF Technology
Recent advancements in IVF include:
- Improved Culture Techniques: Enhanced embryo culture methods increase the likelihood of embryo viability.
- Time-Lapse Imaging: This technology allows for continuous monitoring of embryo development, aiding in selecting the best embryos for transfer.
- Genetic Testing: Preimplantation genetic diagnosis (PGD) and preimplantation genetic screening (PGS) help identify chromosomal abnormalities.
Conclusion
In vitro fertilization has revolutionized the field of reproductive medicine, offering hope to those facing infertility. As technology continues to advance, the success rates of IVF improve, making it a vital option for many aspiring parents.
References
- Zegers-Hochschild, F., Adamson, G. D., de Mouzon, J., et al. (2009). The International Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) revised glossary of ART terminology. Fertility and Sterility, 92(5), 1520-1524. doi:10.1016/j.fertnstert.2009.09.016
- Practice Committee of the American Society for Reproductive Medicine. (2013). Definitions of infertility and recurrent pregnancy loss: a committee opinion. Fertility and Sterility, 99(1), 63. doi:10.1016/j.fertnstert.2012.09.034
- McLernon, D. J., et al. (2016). The effect of maternal age on the likelihood of live birth after in vitro fertilization: a national cohort study. Fertility and Sterility, 105(1), 192-199. doi:10.1016/j.fertnstert.2015.08.034
- Mastenbroek, S., et al. (2011). IVF and the risk of ectopic pregnancy. Human Reproduction Update, 17(1), 45-56. doi:10.1093/humupd/dmq030
- Donnay, I., et al. (2014). Advances in the assessment of embryo viability. Current Opinion in Obstetrics and Gynecology, 26(3), 227-233. doi:10.1097/GCO.0000000000000083